Basic principles
Recent advances in ultrasound technology have led over several years to the development of elastography. This is the ultrasound equivalent of clinical palpation. There are different types of shear elastic properties which can be assessed by ultrasound. Several types have developed using different deformation forces and different ways of measuring the force. A dynamic force (physical pressure, physiological pressure (arterial pulsation), or ultrasoinc propagation is applied and the resulting deformation assessed. An elastogram is measured/displayed in one of three ways:
- Map and measurement of tissue displacement known as ARFI (acoustic radiation force imaging). .
- Strain elastography represent axial displacement measurements on sequential imaging. SEE SONOELASTOGRAPHY THYROID below
- Transient elastography which measure tissue displacement velocities and is used for either FIBROSCAN (no imaging) and shearwave elastography which also includes 2D and 3D imaging. SEE SHEARWAVE LIVER below
For more information about elastography see guidelines from the European Federation of Ultrasound in Medicine and Biology.
Shearwave Elastography of the Liver*
Accurate diagnosis and staging of liver fibrosis is essential for the prognosis and management of chronic liver diseases. Conventional B-mode ultrasound provides only anatomical information. When combined with shear wave technology it can now evaluate stiffness values in patients with liver fibrosis.
In the assessment of chronic HCV hepatitis, the most reproducible biopsy scoring system is the Metavir. On the Metavir scoring system[1], liver fibrosis is evaluated semi-quantitatively and staged on a five-point scale from 0 to 4. F0: absent; F1: enlarged fibrotic portal tract; F2: peri-portal or initial portal-portal septa but intact architecture; F3: architectural distortion but no obvious cirrhosis; and F4: cirrhosis.
With increasing fibrosis, the liver becomes stiffer, which can be monitored using shear wave elastography. A region of interest (ROI) is placed in an area of the right lobe of liver and and several measurements are taken while the patient suspends respiration and a report is generated. The average of these measurements is then used to estimate the degree of liver stiffness and the reliability of the measurement.
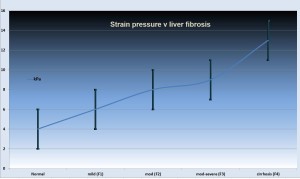
This can be used to estimate the degree of fibrosis. The relationship with a biopsy Metavir score is shown in the figure (right).
Elastography has also been used in fatty liver disease for staging and assessment of fibrosis, see Yoneda et al in Transient elastography in patients with non‐alcoholic fatty liver disease.
Here is a brief video on LIVER elastography.
Most of the early work was done using transient elastography that many of you will know as “fibroscan”. While the techniques in vitro are equivalent, shearwave elastography is real time and has the benefit of visualizing and selecting small samples of liver parenchyma (avoiding vessels, portal triads, etc). Recent studies suggest shearwave has a lower failure rate and a greater accuracy, but is less proven in clinical trials. In Figure 1 the relationship between fibrosis and elastographic index are shown and it should be noted that the intermediate grades of biopsy result have a large overlap in results, which most likely reflect the nature of liver biopsy classification and the patchiness of disease rather than the reproducibility of elastography.
There are many studies looking at the role of elastography in different conditions and there are a number of specific findings for each condition, which include specific cut-off points indicating fibrosis. These vary slightly depending on the study and disease and therefore the absolute levels will have different clinical significance in different clinical settings. Most of these can be found in this excellent overview by Woo Kyoung Jeonget al: Principles and clinical application of ultrasound elastography for diffuse liver disease, Ultrasonography 33(3), July 2014, p149-160.
Clinical applications are widespread and growing as this technique is currently the only reliable quantitative and non-invasive method of assessing hepatocellular damage. Currently it is being used in:
- Chronic viral hepatitis (hepatitis B and hepatitis C) -for diagnosis of fibrosis and cirrhosis
- Other chronic hepatitis
- Fatty liver with hepatitis (NASH and NAFLD)
- Monitoring for drug toxicity (e.g. methotrexate)
- Alcoholic liver diseases
- Liver transplantation
- Portal hypertension
Other possibilities include progress assessments in intervention related to Fatty liver disease and other causes of liver dysfunction. Elastography has been used to predict the development of variceal bleedingusing the the liver stiffness-spleen diameter to platelet ratio score (LSPS) = the product of liver stiffness and the maximum spleen diameter divided by the platelet count. A result of >6.5 prophylatic treatment for bleeding should be considered.
Sonoelastography thyroid*
Elastography is useful in assesing thyroid nodules. For example in calcified nodules, for which B-mode (gray scale) ultrasound has low specificity (i.e., 8.9%) in detecting malignancy, elastography can asses and subsequently exclude about 1/3rd of these from biopsy by confidently classifying them as benign.
Elastography can be considered as a reliable screening tool for characterizing thyroid nodules. An elasticity score of 1 is indicative of benign pathology in almost all cases and can be used to exclude many patients from further invasive assessments[2]. For more about thyroid nodules see Thyroid FNA.
[1] Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology. 1996;24(2):289-93.
[2] Ghhajarzadeh M, Sodagari F, & Shakiba M: Diagnostic Accuracy of Sonoelastography in Detecting Malignant Thyroid Nodules: A Systematic Review and Meta- Analysis. AJR 2014; 202:W379–W389 .