Lung scan renaissance
Lung scans fell out of favour with the advent of multislice CT pulmonary angiography (CTPA) which offered a great improvement on the accuracy of lung scans shown by the PIOPED study done in the 1980’s. There is no doubt that CTPA is a readily available test for diagnosing pulmonary embolism. Nuclear technology has also moved on since the PIOPED study and more recent studies from various centres tend to suggest that there is very little difference in accuracy between the two modalities. In practice it is the appropriate use and application of the test that is more important than whether it is CTPA or V/Q lung scanning. The PIOPED II STUDY (New Engl J Med 2006,354:2317) showed the overall sensitivity of CTPA for the diagnosis of pulmonary embolism was 83% and the specificity was 96%. However, these data excluded CT studies that were technically inadequate or un-interpretable . When all the studies are included the sensitivity and specificity fall to 78% and 90% respectively. The positive predictive value was 86% and the negative predictive value was 95%. Most notably the positive predictive value was only 58% when the clinical probability was low. Therefore additional testing is necessary when clinical probability is inconsistent with the scan results.
Wang, Feng MD et al in Clinical Nuclear Medicine July 2009 (Volume 34 – Issue 7 – pp 424-427) concluded V/Q lung scan, perfusion scan combined with CR and CTPA all show high efficacy in diagnosing pulmonary embolism.
In a head to head comparison (all patients had both tests) of CTPA and SPECT-CT lung scans Gutte et al (V/Q SPECT AND LOW-DOSE CT VS MDCT IN PE. J Nucl Med 2009; 50:1987–1992) found SPECT-CT lung scans had a sensitivity of 97% and specificity of 100%. CTPA alone had a sensitivity of 68% and a specificity of 100%.
In a very recent study done at the Charles Gairdner Hospital Perth (Ling et al. Internal medicine Journal 2012;42:1257-1260) they demonstrated that the addition of low dose CT increases the diagnostic yield by providing alternative diagnoses and contributed to a final diagnosis in 36%. Their use of SPECT-CT for the diagnosis of pulmonary embolism had a sensitivity , specificity, and negative predictive values of 93%,100%, and 97% respectively.
Leonard Freeman concluded that lung scans were as effective as CTPA in the diagnosis of pulmonary embolism in 2011 (see also J Nuc Med 2008;49:5-8).
The high indeterminate rate that previously plagued nuclear studies of the eighties and nineties should be a problem of the past. Most studies and sites indicate an indeterminate rate of less than 7% which is as good as the indeterminate rate from CTPA. Further more the radiation dose of V/Q scans is substantially less and it should be the test of choice in the young and in the pregnant woman.Typical doses are as follows:
V/Q lung scan: 1.2 – 2 mSv whole body dose, 0.9 mSv breast dose; 0.2-0.4 mSv foetus dose (pregnant woman)
4 – slice CTPA: 20-50 mSv whole body dose; 20-60mSv breast dose; 0.96 mSv foetus dose (pregnant woman)
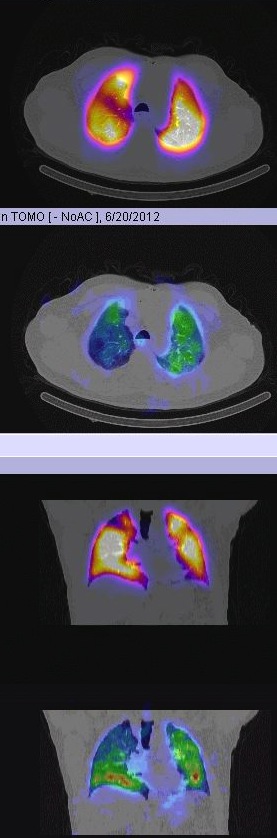
In addition imaging techniques have improved enormously as seen in this perfusion SPECT-CT image of lungs with the colour representing perfusion or in this case of pulmonary embolism using planar or SPECT-CT techniques.
Conclusion
My own experience concurs with the studies above.The indeterminate rate is now much lower and the use of both SPECT and SPECT-CT imaging has further improved the test’s accuracy -most particularly by reducing the indeterminate rate and increasing the test’s specificity. The interpretative algorithms used and report conclusions should be definitive in >90% of cases. In the right clinical context either test can prove or exclude the diagnosis of pulmonary embolism and where one test fails the other should be employed . There are some advantages of using the lower dose V/Q scan in patients with lower probability scenarios or in asymptomatic patients with proven DVT (38% of whom will have a PE). In the acute setting the rapid availability of CTPA makes it appropriate for urgent cases.