 Metatarsalgia and foot pain is a frequent clinical problem and forefoot imaging is undertaken frequently to assist in enabling a more specific diagnosis. Referrals for ultrasound of the forefoot almost always are for the investigation of metatarsalgia and less often for clinical swelling. Most often the referral is looking for the presence of a Morton’s neuroma despite this being one of the least common causes of metatarsalgia. In the author’s experience the refinement of the clinical evaluation prior to ultrasound referral has declined over the last decade and therefore a greater clinical responsibility falls to the sonographer/sonologist team. Both generally in musculoskeletal ultrasound and specifically in the forefoot it is the author’s opinion that sonographers should rise to this challenge and take on greater clinical responsibility. It is insufficient simply to say “no abnormality found” and requires either the sonologist or sonographer give the patient further direction for reaching a diagnosis. This requires the sonographer and sonologist understand the clinical possibilities and diagnostic pathways involved in assessing the forefoot. This article outlines a possible process in the case of the forefoot and provides a general template for this enhanced role. The single biggest advantage diagnostic ultrasound has over other diagnostic modalities is the ability to clinically evaluate the patient and produce highly relevant images. An additional potential benefit is to offer a pathway forward by suggesting the best diagnostic pathway when a specific ultrasound diagnosis cannot be made.
Metatarsalgia and foot pain is a frequent clinical problem and forefoot imaging is undertaken frequently to assist in enabling a more specific diagnosis. Referrals for ultrasound of the forefoot almost always are for the investigation of metatarsalgia and less often for clinical swelling. Most often the referral is looking for the presence of a Morton’s neuroma despite this being one of the least common causes of metatarsalgia. In the author’s experience the refinement of the clinical evaluation prior to ultrasound referral has declined over the last decade and therefore a greater clinical responsibility falls to the sonographer/sonologist team. Both generally in musculoskeletal ultrasound and specifically in the forefoot it is the author’s opinion that sonographers should rise to this challenge and take on greater clinical responsibility. It is insufficient simply to say “no abnormality found” and requires either the sonologist or sonographer give the patient further direction for reaching a diagnosis. This requires the sonographer and sonologist understand the clinical possibilities and diagnostic pathways involved in assessing the forefoot. This article outlines a possible process in the case of the forefoot and provides a general template for this enhanced role. The single biggest advantage diagnostic ultrasound has over other diagnostic modalities is the ability to clinically evaluate the patient and produce highly relevant images. An additional potential benefit is to offer a pathway forward by suggesting the best diagnostic pathway when a specific ultrasound diagnosis cannot be made.
In order to evaluate the patient with a musculoskeletal problem the sonographer can take either a targeted approach eg. look for a neuroma, or systematic (anatomical or clinical) approach eg. evaluate the structures in the region of interest. There are strengths and weakness of both approaches and experienced sonographers will use either or both. These approaches require and understanding of both ultrasound anatomy and clinical possibilities. Understanding all the clinical possibilities (not just those identified on ultrasound) not only enhances the scanning process but allows the sonographer the possibility of suggesting an alternative differential diagnosis by a process of exclusion. Furthermore it is a natural sequel of this general approach to the scanning process that any additional diagnostic steps required will be clear to the sonographer/sonologist and be recommended in the study report and/or directly to the patient.Metatarsalgia can be further refined according to its location or lack of one. The major differential diagnosis is shown below in Table 1. Forefoot Imaging Options
| Diagnosis | Focal | Location | Ultrasound Confirm | Ultrasound Exclude | Alternative Imaging |
| Ganglion | Yes | dorsal | Yes | Yes | MR |
| Tendon rupture | No | Extensor > flexor | Yes | Yes | MR |
| Intermetatarsal bursitis | Yes | IMT | Yes | Yes | MR |
| Morton’s neuroma | Yes | IMT | Yes | Yes | MR |
| Plantar plate injury | Yes | MTP plantar | Yes | Yes | MR > BS > CT |
| Turf Toe1 | Yes | MTP1 | Yes | Yes | MR >BS |
| Fasciitis | Yes | Plantar | Yes | Yes | MR |
| Tendinopathy | Var | Plantar > dorsal | Yes | Yes | MR |
| Tumours | No | Common =giant cell | Yes | No | XR + US/MR |
| Complete fracture | Yes | MT | Yes | No | XR, CT |
| Synovitis | Yes | MTP | Yes | No | BS |
| Arthritis | Yes | MTP | Yes | No | XR, BS, |
| Gout | Yes | MTP> IPJ | Yes | No | BS, MR, +XR/CT |
| Foreign Body | Yes | Plantar | Yes | No | XR,CT |
| Nerve entrapment | No | Tarsal Tunnel Knot of Henry, Medial plantar neuritis |
Yes | No | MR |
| Bone stress injury | Yes | MTH | No | No | BS > MR > XR, CT |
| Infection (bone) | Var | MTH, MTP | No | No | BS>MR |
| Sesamoiditis | Yes | MTH1 | No | No | BS, MRI > CT |
| Freiberg’s infraction | No | MTH2,3 | No | No | MR > BS >XR, CT |
It is clear that most causes of pain have localising features and that it makes sense to start at the site of symptoms in almost all patients. Mostly one can quite quickly either identify (or not) a lesion in the local region. Once a lesion is identified it can be classified according to its location and sonographic characteristics. If a lesion is not identified one then proceeds to rule out other diagnoses that can be excluded by ultrasound (Table 1). At the end of this process there will be a number of diagnoses that cannot be excluded by ultrasound and the most likely of these can be suggested along with further imaging recommendations where appropriate.
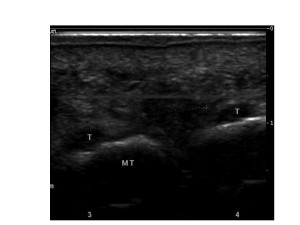
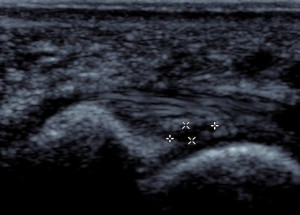
In the case of referral for Morton’s neuroma a brief history should indicate which inter-metatarsal space is primarily of interest and examined. A positive finding in the inter-metatarsal space needs to be characterised further. Though location has been found to be important by some I have found the most useful features differentiating bursitis from Morton’s neuroma to be shape, compressibility, and the relationship of any lesion to the MTP joints and interdigital nerve. A Morton’s neuroma (see figure 1) may be mobile but is not compressible or deformable (moves as a single unit), can be seen in continuity with the nerve (see at upper right of lesion in Figure 1), has a more uniform echogenicity, and has no relationship with the joint.
Bursitis (see figure 2) is compressible, deformable, more heterogeneous in echogenicity, a variety of shapes, sizes, and locations and often has a close relationship with one of the metatarsophalangeal joints (and may communicate with it thought this is often difficult to prove with images). Beware that neuromas and bursitis can coexist in the same patient and appear to occur together much more frequently than expected by chance alone -suggesting some common aetiological factors.
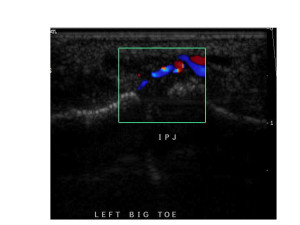
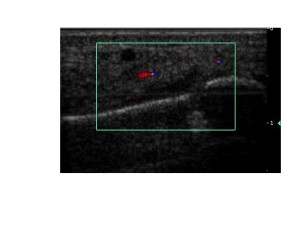
Other common findings include synovial thickening in one or more metatarsophalangeal joints -usually relevant, joint effusions -sometimes relevant, and stress fractures -always relevant. Abnormal blood flow in synovium correlates well with more aggressive synovitis of any cause (see figure 3).
Stress fractures that can be seen with ultrasound are usually proximal to the metatarsal head and are recognised by cortical disruption, abnormal local vascularity (within and around bone), and callus formation (see figure 4). Stress injuries to the metatarsal heads usually have no ultrasound findings other than local tenderness. Some ultrasound findings may be non-specific -joint, tendon, and ligament swellings but are helpful in either pursuing a more specific diagnosis or initiating management.
If no lesion is seen one extends the exam to the adjacent inter-metatarsal spaces and adjacent metatarso-phalangeal joints. In addition one can almost always image the interdigital nerve and show it is of normal appearance. During the scan process one can generally find a focus of maximum tenderness that should raise the level of diagnostic suspicion for lesions at or close to that location. If no ultrasound pathology is found one has usually come down to a differential diagnosis largely based on clinical findings (Table 1).
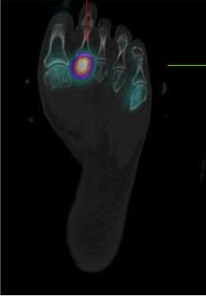
Most often a negative examination in this context leads to a differential diagnosis of bone stress injury or fracture of the metatarsal head (see figure 5) or joint pathology -though usually the latter has findings on ultrasound.
A similar presentation to a metatarsal head stress injury might however have a positive finding on ultrasound such as an adventitial bursitis under the metatarsal head –shown in figure 6.
It is important to try and differentiate between tenderness of the metatarsal head, the adjacent joint, and the base of the proximal phalanx (though this is not always possible). The flexor tendon often overlies all of these structures but ultrasound assisted palpation can often separate the tendon by approaching the bone obliquely. If the tenderness if over the distal inferior part of the joint or at the base of the proximal phalanx one needs to carefully examine the plantar plate and more proximal flexor tendon. It is important to remember a plantar plate abnormality (figure 7) is really only relevant when it is symptomatic. A negative ultrasound associated with focal bone or joint tenderness (and no xray findings) will almost always have a positive bone scan or MRI. In this context SPECT-CT bone scan can almost always give a specific diagnosis. A symptomatic plantar plate injury will also show on higher resolution SPECT-CT or MRI but may not be reported unless specifically queried. The ultrasound has a useful role to either make the diagnosis or to raise suspicion sufficiently that these modalities can be asked to specifically address this diagnosis (positive or negative).
Unusual pathologies occasionally need to be considered when there are no local U/S findings and either a bone scan or MRI show no forefoot abnormality. Top of the list in this scenario are nerve entrapments which can be anywhere from the exiting nerve roots to the distal nerves. Most commonly plantar pain (and sometimes tenderness) can arise from medial plantar nerve entrapment or Tarsal Tunnel syndrome. The latter usually has other clinical clues. Entrapment of the medial plantar nerve (Jogger’s foot) can sometimes be confirmed on ultrasound by seeing an abnormality at the cross-over of flexor digitorum longus and flexor hallucis longus deep to the abductor hallucis (nerve swelling or ganglion) . If the patient has exquisite tenderness at this site but no ultrasound finding then MRI might be suggested to look for nerve entrapment. Tarsal Tunnel syndrome once suspected can be evaluated by examining the tunnel for nerve swelling, cysts, ganglia, etc. Ultrasound in good hands should be able to make or exclude this diagnosis but in any case of high clinical suspicion of nerve entrapment MRI should be recommended for complete evaluation.
Most joint pathology needs to be correlated with x-ray and less often with other modalities. The x-ray also helps with an overview of the skeletal anatomy and many of the lesions discussed above are more common in compromised feet such as primary metatarsus varus and collapsed longitudinal arches. MRI may be required for further evaluation of soft tissue changes and uncertain findings but it is not the modality of first choice for forefoot problems.
By the end of the examination one should either have a definite positive or negative in relation to the clinical question. In the case of a negative one should be able to offer one or more alternative diagnoses and suggest a diagnostic test that could confirm or exclude this.
I thus encourage all sonographers to take a more clinical approach to ultrasound of the forefoot.
References
- Ashman CJ, Klecker RJ, Yu JS. Forefoot Pain Involving The Metatarsal Region: Differential Diagnosis With MR Imaging. Radiographics 2001; 21:1425-40.
- Delfault EM, Demondium X, Bieganski A, Thiron M, Mestdagh H, and Cotton A. Imaging of Foot and Ankle Nerve Entrapment Syndromes: From Well-demonstrated to Unfamiliar Sites. Radiographics 2003;23:613-623.
- Gregg JM, Schneider T, Marks P. MR Imaging And Ultrasound Of Metatarsalgia -The Lesser Metatarsals. Radiol Clin North Am 2008; 46(6):1061-78.
- Zanetti M, Weishaupt D. MR Imaging Of The Forefoot: Morton Neuroma and Differential Diagnosis. Sem Musculoskel Radiol 2005; 9(3):175-186.
Author and Copyright Iain Duncan, 2013.