WHAT IS TENDINOPATHY?
Tendinopathy is a term used for painful conditions occurring in and around tendons in response to injury and/or overuse and ageing. The natural course of symptoms is variable but most ultimately resolve (even if the tendon appearance on scans does not). Generally the length of symptoms varies according to age and severity. A recent study suggested the median length of symptoms was 14 months. The incidence of symptoms in sedentary people is highest in middle age though at particular sites (lateral hips and shoulders) the incidence is greater with increasing age.
HOW IS IT DIAGNOSED?
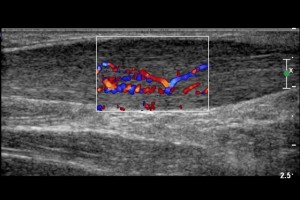
Ultrasound can confirm or rule out the diagnosis but the presence of tendinopathy on ultrasound does not necessarily indicate whether it is the cause of your symptoms. The relationship between symptoms and the scan findings is determined by a clinician who combines the clinical history, examination findings, and all test and scan results. The incidence of asymptomatic tendinopathy also increases with age (i.e. many patients have scan findings of tendinopathy but no real symptoms).
A (well performed) ultrasound or MRI scan will determine whether there are significant tendon tears, inflammation, bursitis, or other nearby soft tissue pathology. It can broadly categorise the type of tendinopathy which usually helps in determining treatment options.
HOW IS IT TREATED?
An ultrasound or MRI scan performed by an experienced operator will determine whether there are significant tendon tears, inflammation, bursitis, or other nearby soft tissue pathology. It can categorise the type of tendinopathy which usually helps in determining treatment options. Commonly used therapies include anti-inflammatory medications, corticosteroid injections, exercise, physical therapy modalities, shock wave therapy, PRP (Platelet rich plasma) injections, sclerotherapy, nitric oxide patches, and surgery. In 2008 there was a systematic review of 177 clinical trials and systematic reviews of the current treatment options the authors made the following conclusions.
“NSAIDS [anti-inflammatory medications] and corticosteroids appear to provide pain relief in the short term, but their effectiveness in the long term has not been demonstrated. We identified inconsistent results with shock wave therapy and physical therapy modalities such as ultrasound, iontophoresis and low-level laser therapy. Current data support the use of eccentric strengthening protocols, sclerotherapy, and nitric oxide patches, but larger, multicenter trials are needed to confirm the early results with these treatments. Preliminary work with growth factors and stem cells is promising, but further study is required in these fields. Surgery remains the last option due to the morbidity and inconsistent outcomes.” 1
Therefore the optimal treatment for tendinopathy remains an ongoing discussion and there are regular studies and ongoing research. Local management will depend on local expertise, individual patient factors, and your own doctor’s experience. Unproven treatment methods are not necessarily ineffective and often practise precedes adequate studies.

NSAIDS and injections are commonly used
Generally, treatment usually starts with a short course of anti-inflammatories and along with physical therapies, this remains the preferred first line of treatment. This should be followed by strengthening exercises and sometimes other physical therapies. Injectable corticosteroids are sometimes used to provide temporary pain relief but studies have generally not shown any longterm benefit and recurrent injections can be harmful. They should not be done where there is a significant tear or risk of tear. However there are some specific scenarios in which they may be beneficial2.
A more recent better quality research has shown promising result with PRP. Platelet rich plasma (PRP) injections have become the injection therapy of choice for recalcitrant tendinopathy which is usually associated with delamination or tears.
Surgical treatment remains the last treatment option but is rarely required.
1. Brett M. Andres MD, George A. C. Murrell. Treatment of Tendinopathy. What Works, What Does Not, and What is on the Horizon. Clin Orthop Relat Res (2008) 466:1539–1554. Published online: 30 April 2008 -The Association of Bone and Joint Surgeons 2008.
2. Johannsen, F., Olesen, J. L., Øhlenschläger, T. F., Lundgaard-Nielsen, M., Cullum, C. K., Jakobsen, A. S., Michael, ;, Rathleff, S., Peter, ;, Magnusson, S., & Kjaer, M. (2022). Effect of Ultrasonography-Guided Corticosteroid Injection vs Placebo Added to Exercise Therapy for Achilles Tendinopathy: A Randomized Clinical Trial. JAMA Network Open, 5(7), e2219661–e2219661. https://doi.org/10.1001/JAMANETWORKOPEN.2022.19661