Bone scans of the spine have become a clinically useful part of the evaluation of back pain. Uptake seen on a SPECT-CT correlates with metabolic activity in bone and the increased resolution and specificity of SPECT-CT has allowed a greater number and variety of clinically relevant findings. Most patients with back pain will have an abnormality on high resolution xSPECT-CT bone scan. Many of these will be clinically relevant and like all bone scans it is sometimes the negative scan that is most helpful.
A recent randomized double blind study by Jain et al1 showed that a bone scan with SPECT-CT improved the clinical workup of patients with low back pain by improving the accuracy of identifying the pain source in a group of 80 patients. The outcome from pain blocks was improved and in a small number of patients it enabled critical diagnoses that changed management entirely.
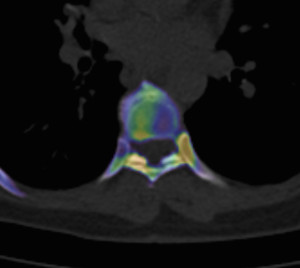
My experience with xSPECT-CT shows that it improves the diagnostic accuracy even further, particularly in relation to thoracic and sacroiliac pain. The image below shows the detail available with xSPECT-CT in the thoracic spine.
The following diagnoses are best made or excluded using a bone scan:
- Active facet joint arthropathy (as opposed to inactive disease which CT and to a lesser extent MRI show anatomic rather than functional changes)
- Significant pars interarticularis fractures (MRI false negative 10%) in young patients
- Fractures
- Bridging osteophytes
- Stress fractures
- Vertebral fatigue fractures
- Boney metastasis (though early lytic disease and lesions less than 5mm are often only seen on xSPECT-CT rather than SPECT-CT)
- In prostate carcinoma suggest bone scan if PSA>10, symptoms, Gleason score >7
- In breast carcinoma suggest bone scan in recurrent breast cancer or stage III,IV disease
- Post surgical fusion complications (>12months post surgery)
- Fusion failure -cold on scans done early post surgery (<8 months) and hot (>18months post surgery)
- pseudarthrosis
- adjacent segment disease
- screw impingement
- Transitional vertebra with partial incorporation stress injuries (not seen generally on MRI)
- Sacroliliitis
- Sacral, coccygeal and pelvic fractures
- Enthesitis at the adductor attachments, greater trochanters,
- Pseudarthrosis between joint variants (partially incorporated vertebra) or between posterior spinous processes
- Heterotopic or dystrophic ossifications
In addition a bone scan is helpful in the investigation of back pain where other imaging is negative, does not correlate with the clinical findings, or has too many abnormalities. It casts a much wider net than either dedicated CT or MRI so has a role in defining poorly localised musculoskeletal pain.
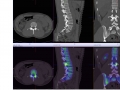
Some typical images:
References:
- Jain, A., Jain, S., Agarwal, A., Gambhir, S., Shamshery, C., & Agarwal, A. (2015). Evaluation of Efficacy of Bone Scan With SPECT/CT in the Management of Low Back Pain: A Study Supported by Differential Diagnostic Local Anesthetic Blocks. Clinical Journal of Pain, 31(12), 1054–1059. https://doi.org/10.1097/AJP.0000000000000212